What are Endotoxins and Exotoxins and where do they come from?

What are Endotoxins and Exotoxins and where do they come from?
The word “toxin” causes my ears and eyes to perk up, because these are the types of substances that cause illness and even death. Thankfully, it is increasingly possible to avoid toxins by understanding where they live and how they’re spread. Science is advancing very rapidly to show us how to manage our environments, food, lifestyle and even our bodies to live more healthfully. Endotoxins come from Gram-negative bacteria, and Exotoxins can come from either Gram-positive or -negative bacteria so we’ll start with what the “Gram” test means.
Bacteria can be classed into two different groups: “Gram-negative” or “Gram-positive”. These classes are based on a test developed by scientist Christian Gram in 1884, which differentiates the bacteria using a purple stain. According to webmd.com, bacteria either have a hard outer shell, or a thick, mesh-like membrane called peptidoglycan. The hard outer shell will resist the purple stain, and show up as a red color. These are called “gram negative” because the purple stain did not show. Bacteria with the peptidoglycan absorb the purple stain much more easily and are called “gram positive”. The stain also tells more characteristics about the bacteria and the way it interacts with treatment.
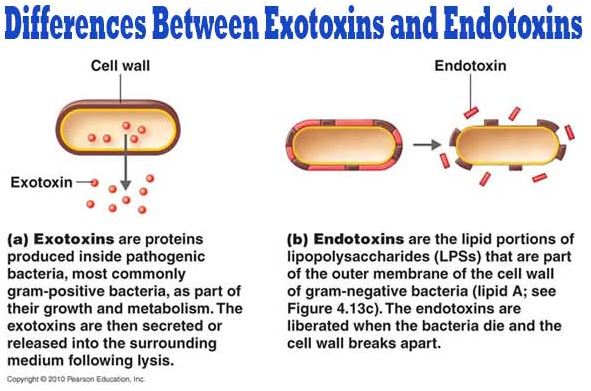
The peptidoglycan layer of Gram-negative bacteria is much thinner than that of gram-positive bacilli; instead Gram-negative have a hard, protective outer shell, making them harder to kill because of their harder cell wall. When their cell wall is disturbed, or the bacteria are dead or dying, gram-negative bacteria release endotoxins that can make symptoms of illness worse. In contrast, exotoxins are produced inside the bacteria and may be released while the bacteria cell is living, or during its death.
Here is a diagram that shows how the exo- and endo-toxins are released (source: microbiologyinfo.com). (I distinguish them by remembering that endotoxins are only emitted at the “end” of life of the bacteria):
Here are some examples of gram-negative bacteria diseases (webmd.com):
- Vibrio cholerae (Cholera, a serious intestinal infection)
- E. coli (E. Coli infection)
- Yersinia pestis (Plague, an infection of the lymph nodes and lungs)
- Bartonella henselae (Cat-scratch disease)
- H. Pylori (gastritis, peptic ulcer disease, gastric lymphoma, and gastric cancer)
- Campylobacter (campylobacteriosis, an infection that usually affects the digestive tract)
- Legionella bacteria (Legionnaire's disease, a lung infection)
- Salmonella (salmonellosis, a digestive infection caused by contaminated food)
Here are some Gram-positive bacteria (and the infections they cause):
- Staphylococcus aureus (MRSA, toxic shock)
- Streptococcus group A (strep throat, toxic shock)
- Clostridium botulinum (botulism)
- Bacillus anthracis (Anthrax)
As you can see, endotoxins and exotoxins are a serious matter! Here are some of the other important differences between them (byjus.com):
Endotoxins |
Exotoxins |
Are released during death, mechanical damage and lysis of bacteria but also during bacterial growth and division. (bmglabtech.com) |
Secreted as part of the cell’s metabolism |
Does not have any enzymatic activities |
Most activities are enzymatic in nature |
Immune response is weaker |
Immune response is stronger |
Made of lipopolysaccharides |
Made of proteins |
Moderately toxic |
Highly toxic |
Cannot be made into toxoids |
Can be made into toxoids |
Highly resistant to heat |
Can be killed by boiling |
(A toxoid is a chemically modified toxin from a pathogenic microorganism, which is no longer toxic but is still antigenic and can be used as a vaccine (Oxford languages).)
There is so much to study about bacteria, however since we at HypoAir mainly focus on air quality, we’ll try to limit this post to the toxins that can be transmitted through the air.
Endotoxins (Endotoxins: Small But Very Significant):
Are pyrogens, that is, they often cause a pyrogenic reaction (fever).
Cause fatigue, a common characteristic of sick building syndrome.
Don’t produce immunity, but only a temporary resistance known as “Monday fever”. Workers in industries with significant endotoxin levels have been found to be most afflicted on Monday, with reduced effects through the week. Endotoxin resistance is lost over the weekend, with the illness beginning anew the following Monday [5]
Are “adjuvant”, meaning that they can amplify the effects of other harmful substances.
Are associated with sepsis, an extreme immune response by the body that often ends in death.
The presence of pets in indoor spaces can represent an important source of air contamination and can be linked with the level of indoor endotoxins. The presence of dogs and cats can be the main predictors of endotoxin levels in house dust [1, 4-7]. Other predictors are the presence of vermin, such as mice, and infrequent cleaning, which indicates poor hygienic conditions in the home [1]. Storage of organic household waste indoors also increases bacterial contamination in the indoor environment [1]. (intechopen.com)
Here are some more details about endotoxins. Although it’s a little in-depth, this article gives a good explanation of what endotoxins are and how they are released (shed) from bacteria. Basically, endotoxins are small molecules of lipopolysacchride (LPS), which comprise approximately 70% of the outer membranes of gram-negative bacteria. They are responsible for maintaining structural integrity and have been shown to be essential for bacterial survival. Lipopolysacccharides vary in their structure, but all share three distinct regions:
O antigen repeats are found on the outermost domain of the LPS molecule and are responsible for host immunogenicity (the ability of the endotoxin to provoke an immune response in human cells).
Core domain is composed of sugars and other non-carbohydrates.
Lipid A is the lipid component of LPS, whose hydrophobicity (repels water) facilitates membrane anchoring. Lipid A is responsible for toxicity of the endotoxin.
Here is a diagram of this structure:
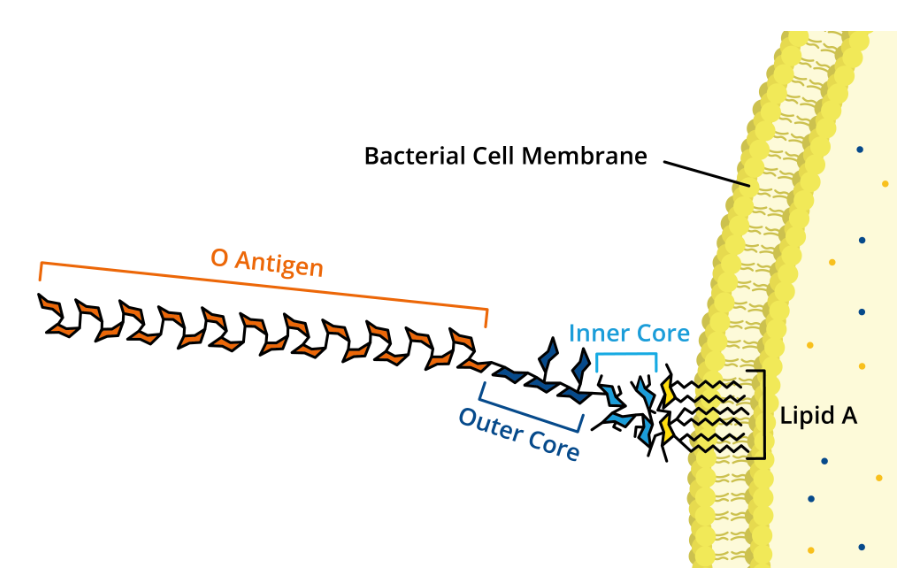
Source: What are endotoxins?
Endotoxins are naturally shed at low levels during bacterial growth, but are released in much larger quantities upon cell death when their cell membranes rupture and disintegrate. A single E. coli cell can release up to 2 million LPS molecules! As lipids, endotoxins are naturally hydrophobic, which gives them a strong affinity for plastics and hydrocarbon-based materials (vinyl flooring, polyurethanes and coatings on many new products).
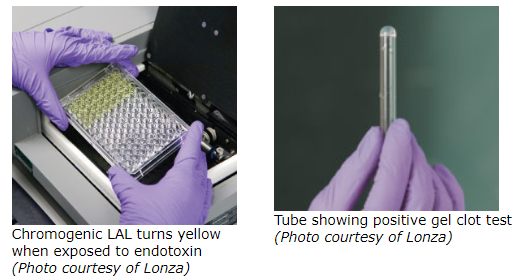
The Limulus Amebocyte Lysate (LAL) test detects endotoxins. It comprises blood cells (amebocytes) from the Atlantic horseshoe crab (Limulus polyphemus) that clot when they encounter bacterial endotoxin lipopolysaccharides. The LAL may be used to test in three different ways: to provide a yes/no (qualitative) answer to whether a sample contains a specified amount of endotoxin, or to obtain the quantity of endotoxin via how fast the clotting takes place (turbidimetric) or how intensely the color changes (chromogenic). (Bacterial Endotoxins Testing) In the qualitative test, equal amounts of a test sample and the gel clot LAL are mixed in a test tube and incubated at 37 °C for 60 minutes. After the incubation, the tube is inverted. If sufficient endotoxin is present in the test sample, the solution would have clotted during the hour incubation and a gel will remain in the bottom of the inverted tube (see image below). If the sample does not contain detectable endotoxin, no clot will form and liquid will run down the side of the inverted tube. (LAL/TAL Endotoxin Detection Test Methods) The enzymatic reaction between the endotoxin and lysate produces a yellow color, the intensity of which is directly linked to the quantity of endotoxin present in the sample.
How can we reduce exposure to endotoxins?
- Reduce Dust: According to EMLab, a commercial IAQ laboratory in North America, “ Endotoxin exposures are mainly through the air.” “Endotoxins do not float freely, but instead are attracted to dust particles. Reduction of dust is essential for controlling endotoxin levels. Dust reduction requires both fresh air filtration and filtered air recirculation. Continuous, low flow fresh air ventilation systems without recirculation do not effectively manage indoor particulates. Endotoxin levels and dust levels are not strongly correlated indicating that they come from independent sources. A single dust particle in the 2 to 10 micron range has sufficient surface area to hold a million or more endotoxin molecules (approximately 0.1ng of endotoxin). Therefore, reduction of dust is important regardless of whether one lives in a dusty or relatively dust-free environment.” (this and following points from buildequinox.com).
- Removal of food sources: “Coupled with proper ventilation is reduction of source generation of endotoxins. In the home environment, it is clear that kitchens are one source of endotoxin generation. Removal of food wastes and standing dishwater will reduce bacterial growth with subsequent production of endotoxins. Even a bowl of standing water will grow bacteria in a home. Bacteria and nutrients are ubiquitous indoors and outdoors, and they will land in water or moist regions where bacterial growth will occur.” Kitchens have the highest level of endotoxins, followed by living rooms and bedrooms.
- Avoid use of misting humidifiers: “Cold temperature (misting) humidifiers are strongly linked to high endotoxin levels. Vaporizing humidifiers that heat water to boiling have not been found to produce high levels of endotoxins.” An alternative method for achieving sanitized, cold temperature humidification in a home is through plant transpiration. Plants can reduce toxins in homes [12]. The plant-root matrix releases sanitized water into the air (assuming proper plant care that does not form a wet mass promoting fungal and bacterial growth).
Exotoxins are (from textbookofbacteriology.net unless otherwise noted)
- part of a defensive system of bacteria to avoid capture and killing by leucocytes (part of our body’s immune system). (sciencedirect.com)
- Produced by both Gram-negative and Gram-positive bacteria
- More highly poisonous by mass than endotoxins, strychnine, or snake venom
- Can be “super-antigenic” or cause stimulation to the immune system
- are often encoded by mobile genetic elements, including bacteriophage (phage). Phage can transfer genetic information to the bacteria they infect. (study)
- Can produce illness even when the microbes that produced them have been killed. (skybrary.aero)
What are the sources of exotoxins? (from intechopen.com)
- Actinobacteria (especially Streptomycetes), Bacillus species and various other bacteria grow in moist building materials together with fungi. Elements from bacterial structures released in air include bacterial cells, bacterial spores, peptidoglycans, microbial volatile organic compounds, exotoxins, and other bacteria growing metabolites.
- Gram-positive bacteria with exo- and endospores like Streptomyces and Bacillus can grow on moist building materials. Their spores are very resistant and can survive even if the air humidity is low.
- Humans are an important source of indoor bacteria. The upmost layer of the normal human skin is continuously renewed, and skin scales containing bacteria are shed into the environment. Bacteria in the respiratory airways are eliminated through Pflügge droplets while talking, coughing, or sneezing. The level of air contamination is dependent on the number of persons inside a room and the efficiency of the ventilation system (natural or artificial ventilation). Bacteria that can be identified in indoor air are micrococci, staphylococci, streptococci, and corynebacteria.
How can we reduce exotoxin exposure?
- Maintain your home so that there are no active leaks and humidity stays between 40-60%. This will reduce actinobacteria that produce exotoxins.
- Practice good hygiene by covering your mouth and nose while coughing or sneezing. This reduces the amount of small particles in the air that can contain bacteria and exotoxins. Dispose of tissues in the trash and wash hands with soap and water.
- According to the WHO, if exposure to the toxin via aerosol inhalation is suspected, additional exposure to the patient and others must be prevented. The patient's clothing must be removed and stored in plastic bags until it can be washed thoroughly with soap and water. The patient should shower and be decontaminated immediately.
- Most exotoxins can be destroyed by heating, (wikidoc.org), so eating thoroughly cooked food often eliminates the danger of ingesting the exotoxin. The WHO recommends these five strategies in food safety:
- keep clean
- separate raw and cooked
- cook thoroughly
- keep food at safe temperatures
- use safe water and raw materials.
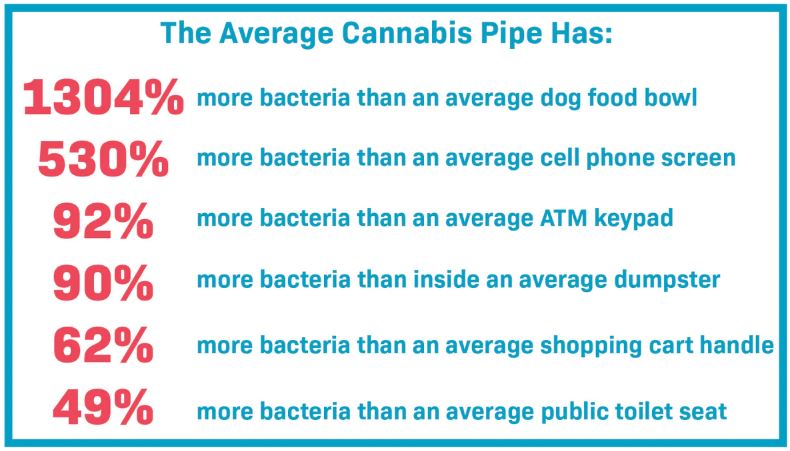
Use of a HEPA filter can reduce aerosols and fine particles containing bacteria, endotoxins and exotoxins, although some of the smaller phages may slip through. This is where a healthy immune system and abstaining from smoking pick up. Cigarette smoking is a substantial risk factor for important bacterial and viral infections. For example, smokers incur a 2- to 4-fold increased risk of invasive pneumococcal disease. (2004 study). In addition, exposure to cigarette smoke causes MRSA bacteria (just one bacteria studied) to become even more resistant to killing by the immune system. (UCSanDiego Health News) Of course, smoking through a dirty water pipe (bong) is inviting disaster! Here are the details (mooselabs.us):
Bacteria, endotoxins and exotoxins are all around us (and even in us), but with good judgment and precautions, you can avoid being one of the infection statistics!